Marie Elwood remembers the night before her med school pulmonology and gas exchange test well.
It was spent sleepless in a Billings, Montana emergency room with her sick infant son. Early the following day, Elwood’s husband—who’d been carrying for the rest of the family—arrived so she could drive straight into her examination.
Though Elwood—a mother of seven and former nurse—admits it wasn’t the highest mark she’s ever received, she cleared another unavoidable obstacle of tackling med school later in life.
“I was just happy with a pass that day—it was one of those things when you have to accept it,” Elwood says.
“All through education, you’re taught to learn for the test, right? In medical school, you’re learning for life. I need to know enough so that I’m a competent physician and serve my patient, not to ace some random test put together by the NBME or something.”

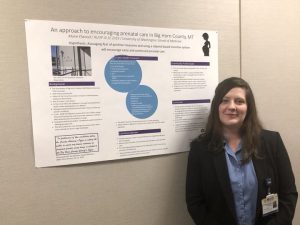
Next month, the 43-year-old will graduate from the University of Washington School of Medicine in Seattle. Last week, she matched as a family medicine resident in Pocatello, Idaho.
Elwood is a member of one of the rarest groups in medical education: those who begin their journey of becoming a doctor later in life.
Statistics showing the breakdown in ages are hard to come by. Still, numbers from the Association of American Medical Colleges (AAMC) show that just 0.3 percent of enrolling medical students between 2000 and 2020 were aged 40 or older.
Elwood started when she was 39. The median age of first-year American med students is 24. Though maturity and understanding gained through life experience help make for a more empathic doctor and colleague, the reality of doing med school later on can be grueling.
Complicated by the Covid-19 pandemic, the demands on her time resulted in countless personal sacrifices for her and her family. The financial pressure of medical student loans hasn’t been avoided, nor have hints of “ageism” as her medical education progressed towards residency.
Yet Elwood’s story is one of inspiration. A domestic abuse survivor, she set up a support group for med school classmates who have suffered from it. And thanks to an effective and forward-thinking rural track program designed to boost the number of physicians serving small towns across the Pacific Northwest, she’s heading into her first-choice residency as the perfect fit for a community, regardless of her journey to get there.
“I think I surprised a lot of people,” she says. “People have different paths, and I feel like I’ll be a very strong doctor based on the experiences I’ve had.”
A dream reborn
Born in Laramie, Wyoming, Elwood grew up in the gold-mining town of Elko, Nevada. Her father was—and remains—a hospital pharmacist there. Through him, Elwood got a job working in medical records when she was 14.
The potential to help people, as a doctor, during some of the most challenging times in their lives just felt right to her.
“The thing I saw was that [physicians] walk beside people, whatever they were going through,” Elwood says. “If that’s death, a cancer diagnosis, or just a difficult time in their lives, the doctor is there and being a force for good.”
The thing I saw was that [physicians] walk beside people, whatever they were going through. If that’s death, a cancer diagnosis, or just a difficult time in their lives, the doctor is there and being a force for good.
By the end of her teens, med school seemed a world away. Elwood gave birth to twin girls when she was 19. Her former partner was physically abusive, leaving a loss of confidence that stuck around long after he had gone.
“I had a rough go of it,” she says. “Any time you’re in an abusive relationship, and you suffer abuse, it will hurt your self-esteem and keep people from accomplishing their potential. It did for me.
“It knocked me back for about ten years before I felt good enough about myself that I could stretch out of my boundaries.”
Slowly but surely, Elwood did. She studied psychology on a pre-med track at the University of Southern California before gaining a Master’s in entomology from the University of Nebraska.
Along with nursing, Elwood got involved in medical research. After moving from Oregon to Montana to be nearer to her husband’s family, she started as a clinical research coordinator for Montana Health Research (MHR), doing work for the FDA. By this time, Elwood says she had “more or less” let go of her teenage dream of becoming a physician.

It wasn’t as if she was heartbroken about it. She enjoyed her work, her personal life was busy but manageable, and there was enough money to go around. Elwood was happy.
In 2017, she told Dr. Michael Hagan—an internal medicine physician she’d check lab values with at MHR—her old dream was unrealistic.
“I said, ‘well, I’m too old, and I’ve got kids,” she says. “He turned around and said, ‘you don’t know how old I was, and I have kids.”
Originally a clinical pharmacist, Hagan was in his late 30s and had two children when he decided to go to med school. “He shot holes in my excuses,” Elwood says.
Elwood took it slow at first, taking the MCAT to see how she’d fare. She did well, so applied to eight med schools across the Northwest. Hagan would write one of her recommendation letters. She was eventually accepted by the UW School of Medicine in Seattle, which she started in 2019.
“. . . the reality is there is no time for that, now.”
In February 2020, Dr. Monya De—a former television reporter turned physician—advocated for beginning med school later in life, arguing that the added maturity, perspective, and potential financial flexibility make for better doctors.
“The axe of autonomy must rip at the root of doctors’ dependence on the fickle medical professional for a career and life satisfaction and financial security,” she wrote. “Medicine should be an individual’s second profession.”
In an ideal world, De’s words ring true. An older student could indeed arrive at med school with teen children and an earlier career or supportive partner that lessens financial or time demands that come with it.
People arrive at that first year of study for many reasons, however. The unique reality of those journeys means the “ideal” set-up is often rare.
Elwood could not avoid taking on substantial loans to complete her medical studies. While hopeful for future federal loan student forgiveness, she says she plans to enroll in Montana’s Rural Physician Incentive Program, a pathway that bonds physicians to clinics in exchange for loan payment from the state.
I thought I would be able to take on med school like my Master’s and still run the house—that has not been the case. Maybe when residency is over, it will be different, but the reality is there is no time for that, now.
But while she understood the financial obstacles she would face before entering med school, her time as a student brought new challenges. Once studying, the difficulty of splitting time between Billings, Seattle, clinical rotations across Montana, and the 24/7 job of being a mom hit home fast for Elwood.
“Maybe I’m generalizing here, but most people who go to medical school are type-A personalities,” Elwood says. “We want to be in charge, and we want to do things our way; we’re a little bossy, right?
“Letting go of some of that perfectionism has been the challenge for me with things like how tidy my house is or how many vegetables and fruits my children are eating all day if I’m not the one doing it.”
After losing his job as physical therapy practice manager when the Covid-19 pandemic began, Elwood’s husband took a lower-paying, less time-consuming position on a pharmaceutical factory line to help better share parental duties.
Recalling the struggle of the pulmonology test after that sleepless night in hospital, Elwood admits there were some moments that pushed both of them to their limits. They got through, she says, and will continue to.
“I thought I would be able to take on med school like my Master’s and still run the house—that has not been the case,” she says. “Maybe when residency is over, it will be different, but the reality is there is no time for that, now.”
Though she says “ageism” wasn’t a big factor at med school or in residency interviews, Elwood admits it would pop up now and then on clerkships.
“It’s stuff like showing up on clerkships and the clerkship director saying ‘who are you?’ and I’ll have to say I’m a med student,” she says.
“It’s more from patients, really. But it’s good, really—I’m breaking down the preconception of what someone in this space should look like.”
The final steps
Despite the sacrifices and challenges, the uniqueness of Elwood’s journey has benefited many people besides just herself.
While at the UW School of Medicine, Elwood co-founded the Divorce and Domestic Abuse Coalition, a group that provides support for med students who have experienced domestic violence. She says she found that “around one in ten” of her fellow med students had experienced some form of domestic violence.
With help from Montana’s Targeted Rural Underserved Track (TRUST) program, which enables aspiring rural physicians to complete clinical rotations in underserved communities, Elwood was able to get her first taste of medicine outside nursing. Her upcoming residency in Pocatello will see that continue.
Rural Americans have access to an average of 39.8 physicians per 100,000 residents. In comparison, there are around 53.3 physicians for every 100,000 urban Americans.
Since TRUST began in Montana in 2008, 110 rural med students have become physicians. The program has grown rural doctors across the Pacific Northwest.
You might as well go for it. As medicine becomes more inclusive, it’s going to be great to see what different things different people can bring to the table.
In spending more time with rural communities, Elwood says she has learned much about the importance of coordinated/collaborative care for non-urban patients. Keeping patients “where they want to be” as much as possible is key.
“It’s important that a patient who breaks their leg in Baker, Montana gets the same care as someone who does the same thing in Seattle, Washington,” she says.
Elwood’s upcoming Pocatello residency will see her family relocate for most of the next three years. Her husband and at least four of their children will come with her.
Residency is likely to provide many more challenges for them all, but reflecting on her medical path, Elwood says she’s happy with how it has unfolded. Med school came along at the right time for her. Her advice for those considering it a little later in life is that it might be for you, too.
“We’re living longer and longer—I honestly plan on working until I’m 90,” Elwood says.
“That’s a long time not doing what you want to do. You might as well go for it. As medicine becomes more inclusive, it’s going to be great to see what different things different people can bring to the table.”